In my last post, we explored the current state-of-the-art of the Enterprise Imaging (EI) industry. In this post, I will zoom in on storing and managing non-DICOM images and videos. This can be ambiguous and may confuse providers who are trying to procure an EI solution. It also results in different schools of thought among vendors.
Currently, EI content can be stored and managed in one of the following formats:
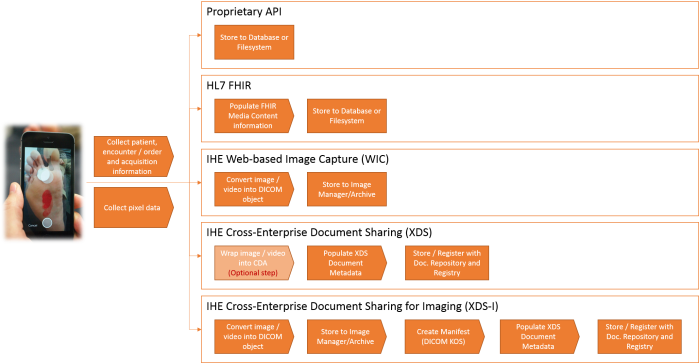
- Original object (e.g. jpg) stored in a solution’s database and/or filesystem using the vendor’s API (Application Programming Interface)
- Original object (e.g. jpg) stored using the IHE Cross-Enterprise Document Sharing (XDS) integration profile in a solution’s XDS Document Repository component
- Original object (e.g. jpg) stored in a solution’s database and/or filesystem using HL7’s FHIR® Media Content specifications
- DICOM object stored in a solution’s Image Manager/Archive component; for example, using the IHE Web Image Capture (WIC) integration profile
- DICOM object stored in a solution’s Image Manager/Archive and XDS Document Repository components using the IHE Cross-Enterprise Document Sharing for Imaging (XDS-I) integration profile
The following diagram depicts the main steps that take place during information capture activity for each method.
All of the above methods have corresponding pros and cons, which leads to the current divergence of opinions regarding the best option to use. Having said that, it is clear that, irrespective of the chosen method, there is a need to properly collect and manage patient, administrative and clinical context (aka metadata) for the acquired EI content.
Metadata
Each of the above methods offer different levels of metadata rigidity and extensibility which impact the interoperability:
- DICOM, FHIR and XDS-I based methods offer a level of certainty for the vendors with respect to what information should be captured and how it should be encoded.
- XDS takes an approach of developing specific content profiles that address specific types of content; for example, the IHE XDS-SD (Scanned Document) integration profile. At the moment, there is no content profile that is specific to the Enterprise Imaging domain. Additionally, XDS allows the original object to be wrapped in a CDA Document to capture additional metadata in case the specified XDS Document Entry attributes are not sufficient.
Is there one “right” answer?
There are two overarching clinical reasons to capture EI content:
- To enrich patients’ clinical record
- To provide reliable, authorized access to it across the enterprise (and beyond)
As the following diagram suggests, the way EI content is stored is less important then the flexibility of an EI solution’s “Capture” and “Discovery and Access” components, because it is hidden behind those interfaces.
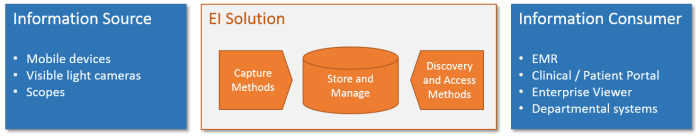
It seems that, currently, there is no single answer for the best EI content format given the informatics complexity of healthcare provider’s enterprises. In order to adapt and compete, vendors will be pressured to support multiple inbound and outbound methods (such as FHIR, DICOM, DICOMWeb, XDS, proprietary APIs, etc.) and only time will tell which approach will become a de-facto standard.
Working on an Enterprise Imaging project? Leave us a comment with your thoughts, or contact us.