When I discuss industry trends with colleagues and clients, I find that we periodically touch on the topic of defining and realizing VNA and Enterprise Viewer (EV) projects’ return on investment (ROI). Our industry has made several attempts to develop an ROI calculator, which would typically encompass:
- the benefits of consolidating IT infrastructure;
- avoiding the cost of repeat exams due to the availability of a longitudinal patient imaging record;
- and efficiency gains stemming from the optimized distribution and visualization of medical images.
Often these calculations are tied to a specific project and not easily reused.
During our involvement in various VNA and EV projects, we observed an interesting pattern that can bring an additional perspective on the ROI discussion.
By the end of 2010, the vast majority of U.S. hospitals had installed a PACS solution. The bulk of the deployments took place during the 2005-2010 period, and many of those are still in place, bolstered by many upgrades and technology-refresh cycles since their initial installations. During that period, both the hardware and storage components of a PACS solution were often procured directly from the PACS vendors. This procurement approach allowed the vendors to enjoy significant Service and Maintenance Agreement (SMA) revenues that would cover not only their solution components but also any included third-party hardware and storage.
Since that procurement wave, many things have changed:
- PACS market maturity resulted in a commoditization of some of its functional areas
- Hardware and storage costs have significantly dropped
- Server virtualization became the preferred deployment methodology
- Procurement of the infrastructure components has been steadily shifting from the Radiology department to the Enterprise/Corporate IT team
Also, PACS market saturation depreciated PACS vendors’ software license sales, resulting in SMA revenues becoming the key contributor to their top line.
All of these changes often created a tension between a hospital’s staff and its PACS vendor because the perceived value of the services delivered under the SMA contracts do not seem to warrant the high dollar cost. Besides tough negotiation tactics, a hospital has few practical tools at its disposal to change this dynamic. This is where well-thought-out VNA and EV projects may become extremely important in changing the negotiation power balance.
The technical and operational benefits of having a VNA take over a PACS Archive, EMR integration and sometimes even workflow components by the VNA and EV solutions are well documented and often result in the hospital’s reduced dependency on the existing PACS vendor.
Consequently, a hospital that implements VNA and EV solutions will be well-suited to renegotiate existing PACS SMA contracts to adequately reflect the provided service. The reduced SMA value can partially offset the cost of VNA and EV projects, thus contributing positively to the ROI calculation. Having said that, without a compelling event, such as an RFP to replace the existing PACS, the incumbent vendor will have little incentive to concede in the SMA renegotiations.
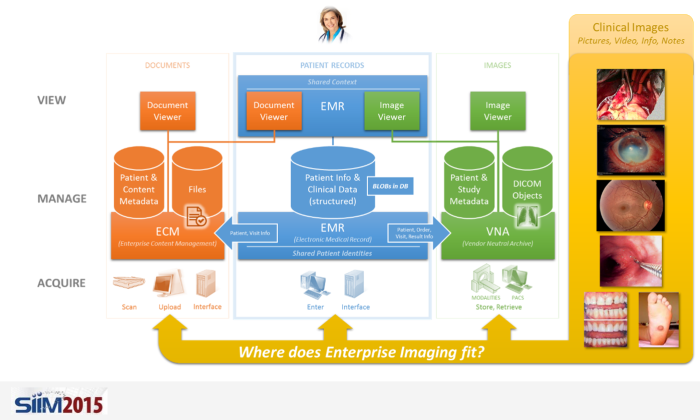
In order to successfully realize the above potential savings, it is important to understand what core functional areas of a PACS can be replaced by a VNA or an EV solution. Consider the following diagram:

| Impact on Workflow or External Systems | Replacement Complexity | Industry Ability to Replace | |
| Long-term Archiving and ILM | This functionality is typically not exposed to external systems and has relatively simple orchestration workflows | Low: Besides the need to keep the VNA copy of the study in sync with the one cached by the PACS, the archival and retrieval functionality is relatively straight-forward | Current state-of-the-art VNA solutions offer proven methodologies to take over this functional area from the PACS |
| Routing, Pre-fetching and Relevancy | This functional area may play an important role in orchestrating a departmental or an enterprise workflow | Moderate: Relevancy detection can potentially increase the relative complexity of study routing and pre-fetching, which are typically quite straightforward due to their transactional nature | The majority of the leading VNA solutions can adequately deliver this functionality, but their rule-definition flexibility coupled with their ability to express sophisticated relevancy rules (especially across multiple terminology domains), may vary |
| Acquisition and Quality Control (QC) Workflow Orchestration | This functionality has a major impact on the acquisition and reading workflow with a large number of 3rd party systems integrations | High: The large number of acquisition modalities will often have different associated configurations. Additionally, in large enterprises QC workflows could be very complex involving both automatic and manual activities. The effort to recreate all QC workflows, which were accumulated over the course of many years could be quite significant | The VNA systems’ ability to provide this functionality represents one of the major product differentiation areas among current vendors |
| Image Distribution and EMR Integration | An ability to provide access to images outside of the Radiology department is a critical component of a provider’s single patient record objective | Low: The need to provide access to images within multiple applications (e.g. EMR, portal) or stand-alone impose some security and integration challenges. Besides the privacy and security considerations, the rest of the deployment and integration activities are relatively straight forward. | Current state-of-the-art EV solutions offer proven methodologies to take over this functional area from PACS |
Although this post is primarily focused on SMA-related costs, the reduction of the PACS functional scope will also decrease the corresponding Professional Services expenses.
Working on an Enterprise Imaging project? Leave us a comment with your thoughts, or contact us.